Pterygium | Ophthalmology
A pterygium (from the Greek, pterygos, “little wing”) is a wing-shaped, vascular, fleshy growth that originates on the conjunctiva and that can spread to the corneal limbus and beyond. Pterygia are relatively common in the general population and typically follow an indolent course, with changes in appearance but little effect on vision and the eye itself. Because early pterygia are usually asymptomatic, there has been little research on their natural history and treatment, and most ophthalmologists commonly consider them an insignificant problem until the lesions encroach on the visual axis. There has been no consensus on the appropriate management of pterygia.
Morphology
A pterygium consists of three distinct parts: the cap, the head and the body/tail.
The cap or leading edge is a flat zone on the cornea that consists mainly of fibroblasts that invade and destroy Bowman’s membrane.
The head is a vascular area that lies behind the cap and is firmly attached to the cornea.
The body/tail is the mobile area of the bulbar conjunctiva, which can be easily dissected from the underlying tissue.1
Stocker’s line, which is iron deposition in the basal layer of corneal epithelium anterior to the cap, indicates that the pterygium is chronic.
Etiology and Pathogenesis
There is a host of theories attempting to explain the pathogenesis of a pterygium; however, the etiology has yet to be determined. Most studies have shown a geographical variation in incidence, with countries closer to the equator showing higher rates of occurrence.
A leading theory proposes that the increased prevalence of pterygium among people in equatorial regions is due to the damaging effects of ultraviolet radiation, specifically UV-B radiation. The working hypothesis is that this radiation causes mutations in the p53 tumor suppressor gene, thus facilitating the abnormal proliferation of limbal epithelium.
Symptoms
Early in the disease process, pterygia are usually asymptomatic; however, there can be signs of dry eye (such as burning, itching or tearing) as the lesion causes irregular wetting of the ocular surface.
As the disease progresses, the lesion increases in size and becomes more apparent to the naked eye and may become cosmetically unpleasant for the patient. Further growth may cause visual symptoms due to induced astigmatism or direct encroachment onto the visual axis.
Treatment
Surgical techniques. The main challenge to successful surgical treatment of pterygium is recurrence, evidenced by fibrovascular growth across the limbus onto the cornea. Many surgical techniques have been used, though none is universally accepted because of variable recurrence rates. Regardless of the technique used, excision of the pterygium is the first step for repair. Many ophthalmologists prefer to avulse the head from the underlying cornea. Advantages include quicker epithelialization, minimal scarring and a resultant smooth corneal surface.1
The bare sclera technique involves excising the head and body of the pterygium while allowing the bare scleral bed to re-epithelialize. High recurrence rates, between 24 percent and 89 percent, have been documented in various reports.
A conjunctival autograft technique has recurrence rates reported to be as low as 2 percent and as high as 40 percent in several prospective studies. The procedure involves obtaining an autograft, usually from the superotemporal bulbar conjunctiva, and suturing the graft over the exposed scleral bed after excision of the pterygium. Complications are infrequent, and for optimal results Stark and coworkers3 stress the importance of careful dissection of Tenon’s tissue from the conjunctival graft and recipient bed, minimal manipulation of tissue and accurate orientation of the graft. Lawrence W. Hirst, MBBS, from Australia recommends using a large incision for pterygium excision and a large graft and has reported a very low recurrence rate with this technique.4
Amniotic membrane grafting has also been used to prevent pterygium recurrence. Although the exact mechanism by which the amniotic membrane confers its beneficial effect has not yet been identified, most researchers have suggested that it is the basement membrane that contains factors important for inhibiting inflammation and fibrosis and promoting epithelialization. Unfortunately, recurrence rates vary widely among the studies that exist, somewhere between 2.6 percent and 10.7 percent for primary pterygia and as high as 37.5 percent for recurrent pterygia.1 A distinct advantage of this technique over the conjunctival autograft, however, is the preservation of bulbar conjunctiva. Amniotic membrane is typically placed over the bare sclera, with the basement membrane facing up and the stroma facing down. Some recent studies have advocated the use of fibrin glue to help the amniotic membrane graft adhere to the underlying episcleral tissue. Fibrin glue has also been used in conjunctival autografts.
Видео Pterygium | Ophthalmology канала Knowing Anatomy
Morphology
A pterygium consists of three distinct parts: the cap, the head and the body/tail.
The cap or leading edge is a flat zone on the cornea that consists mainly of fibroblasts that invade and destroy Bowman’s membrane.
The head is a vascular area that lies behind the cap and is firmly attached to the cornea.
The body/tail is the mobile area of the bulbar conjunctiva, which can be easily dissected from the underlying tissue.1
Stocker’s line, which is iron deposition in the basal layer of corneal epithelium anterior to the cap, indicates that the pterygium is chronic.
Etiology and Pathogenesis
There is a host of theories attempting to explain the pathogenesis of a pterygium; however, the etiology has yet to be determined. Most studies have shown a geographical variation in incidence, with countries closer to the equator showing higher rates of occurrence.
A leading theory proposes that the increased prevalence of pterygium among people in equatorial regions is due to the damaging effects of ultraviolet radiation, specifically UV-B radiation. The working hypothesis is that this radiation causes mutations in the p53 tumor suppressor gene, thus facilitating the abnormal proliferation of limbal epithelium.
Symptoms
Early in the disease process, pterygia are usually asymptomatic; however, there can be signs of dry eye (such as burning, itching or tearing) as the lesion causes irregular wetting of the ocular surface.
As the disease progresses, the lesion increases in size and becomes more apparent to the naked eye and may become cosmetically unpleasant for the patient. Further growth may cause visual symptoms due to induced astigmatism or direct encroachment onto the visual axis.
Treatment
Surgical techniques. The main challenge to successful surgical treatment of pterygium is recurrence, evidenced by fibrovascular growth across the limbus onto the cornea. Many surgical techniques have been used, though none is universally accepted because of variable recurrence rates. Regardless of the technique used, excision of the pterygium is the first step for repair. Many ophthalmologists prefer to avulse the head from the underlying cornea. Advantages include quicker epithelialization, minimal scarring and a resultant smooth corneal surface.1
The bare sclera technique involves excising the head and body of the pterygium while allowing the bare scleral bed to re-epithelialize. High recurrence rates, between 24 percent and 89 percent, have been documented in various reports.
A conjunctival autograft technique has recurrence rates reported to be as low as 2 percent and as high as 40 percent in several prospective studies. The procedure involves obtaining an autograft, usually from the superotemporal bulbar conjunctiva, and suturing the graft over the exposed scleral bed after excision of the pterygium. Complications are infrequent, and for optimal results Stark and coworkers3 stress the importance of careful dissection of Tenon’s tissue from the conjunctival graft and recipient bed, minimal manipulation of tissue and accurate orientation of the graft. Lawrence W. Hirst, MBBS, from Australia recommends using a large incision for pterygium excision and a large graft and has reported a very low recurrence rate with this technique.4
Amniotic membrane grafting has also been used to prevent pterygium recurrence. Although the exact mechanism by which the amniotic membrane confers its beneficial effect has not yet been identified, most researchers have suggested that it is the basement membrane that contains factors important for inhibiting inflammation and fibrosis and promoting epithelialization. Unfortunately, recurrence rates vary widely among the studies that exist, somewhere between 2.6 percent and 10.7 percent for primary pterygia and as high as 37.5 percent for recurrent pterygia.1 A distinct advantage of this technique over the conjunctival autograft, however, is the preservation of bulbar conjunctiva. Amniotic membrane is typically placed over the bare sclera, with the basement membrane facing up and the stroma facing down. Some recent studies have advocated the use of fibrin glue to help the amniotic membrane graft adhere to the underlying episcleral tissue. Fibrin glue has also been used in conjunctival autografts.
Видео Pterygium | Ophthalmology канала Knowing Anatomy
Показать
Комментарии отсутствуют
Информация о видео
Другие видео канала
 Paranasal Air Sinus and Frontal Air Sinuses | Anatomy | Functions | Clinical
Paranasal Air Sinus and Frontal Air Sinuses | Anatomy | Functions | Clinical INCONTINENCE or ENURESIS - Symptom
INCONTINENCE or ENURESIS - Symptom Obturator Externus - Muscle | Origin | Insertion | Nerve supply | Actions
Obturator Externus - Muscle | Origin | Insertion | Nerve supply | Actions Abscess
Abscess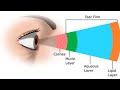 Components of Tear Film | Ophthalmology
Components of Tear Film | Ophthalmology Adductor Brevis - Muscle | Origin | Insertion | Nerve supply | Action
Adductor Brevis - Muscle | Origin | Insertion | Nerve supply | Action Pertussis (Whooping cough) | Pathology | Epidemiology | Treatment
Pertussis (Whooping cough) | Pathology | Epidemiology | Treatment Rinne's test | Tuning Fork Tests - ENT
Rinne's test | Tuning Fork Tests - ENT Gelles Test | Tuning Fork Test | ENT
Gelles Test | Tuning Fork Test | ENT Blood Supply of Facial Nerve
Blood Supply of Facial Nerve Trichomonas Vaginalis / Trich Infection
Trichomonas Vaginalis / Trich Infection Absolute Bone Conduction Test (ABC) | Tuning Fork Test | ENT
Absolute Bone Conduction Test (ABC) | Tuning Fork Test | ENT Weber Test Tuning Fork Test ENT
Weber Test Tuning Fork Test ENT Differences between Nephrotic and Nephritic Syndrome
Differences between Nephrotic and Nephritic Syndrome Kyphosis - Medical symptomatology | Types and Causes
Kyphosis - Medical symptomatology | Types and Causes Histology of Vas Deferens \ Ductus Deferens
Histology of Vas Deferens \ Ductus Deferens Subclavius - Muscle | Origin | Insertion | Nerve supply | Anatomy
Subclavius - Muscle | Origin | Insertion | Nerve supply | Anatomy Superior and Inferior Mesenteric Veins | Venous Drainage of small intestine
Superior and Inferior Mesenteric Veins | Venous Drainage of small intestine Interoceptors and Receptors | Physiology | Types and Fibers Part-2/3
Interoceptors and Receptors | Physiology | Types and Fibers Part-2/3 Important Lower Limb Questions | Anatomy Examination
Important Lower Limb Questions | Anatomy Examination