Incidental pancreatic cysts - what we know and what we don't know, Jay Heiken
http://www.icimagingsociety.org.uk/
Pancreatic cysts are very common in the adult population, and the prevalence increases with age. Pancreatic cysts are identified in 13%-20% of adults undergoing abdominal magnetic resonance imaging (MRI) [1, 2] and in 2.6% of individuals undergoing multi-detector CT [3]. How we deal with these cystic lesions has important implications for both patient care and the expenditure of healthcare dollars.
Most pancreatic cysts discovered incidentally on imaging studies are branch duct intraductal papillary mucinous neoplasms (BD-IPMN). The vast majority are larger than 3cm and have a very low risk of malignancy [4]. Nevertheless, certain imaging features of pancreatic cysts are associated with an increased risk of malignancy. The international consensus guidelines for the management of pancreatic mucinous neoplasms [4] identify a group of features which are characterized as “worrisome features” (size larger or equal to 3 cm, thickened enhanced wall, main pancreatic duct (MPD) size 5-9 mm, non-enhanced mural nodule(s), abrupt change in MPD caliber with atrophy of the upstream pancreas, and lymphadenopathy) and “high-risk stigmata” (obstructive jaundice in a patient with a pancreatic head lesion, enhanced solid component, and MPD size larger or equal to 10 mm).
Recent surgical data indicate that individuals with pancreatic cysts may be at increased risk of developing solid pancreatic neoplasms. 4%-10% of patients with resected BD-IPMN are found to have concurrent pancreatic ductal adenocarcinoma [5, 6]. In addition, patients with one or more pancreatic cysts have an increased risk of subsequent development of pancreatic ductal adenocarcinoma [7, 8].
Whether individuals with multifocal BD-IPMN are at increased risk of malignancy is unclear. Although most studies have not shown an increased risk of malignancy compared with solitary BD-IPMN, on study found that in 52 patients with larger or equal to 4 pancreatic cysts, 34% had high grade dysplasia or invasive carcinoma and 17% had a coexistent ductal adenocarcinoma [9].
Almost all of the data available on the biological behavior of pancreatic cysts come from surgical series and longitudinal imaging studies. No randomised controlled trials have been performed. Therefore our approach to the management of incidentally discovered pancreatic cysts is based on consensus guidelines developed by panels of medicine, surgery, pathology and imaging experts [4, 10, 11], and there is still a great deal to be learned about the genetics, natural history and risks associated with these cysts.
All of the consensus guidelines recommend that a cyst larger or equal to 3 cm should be followed as long as it contains no worrisome or high-risk features; however, what the follow-up schedule should be and when surgical intervention is indicated varies among the guidelines. Most consensus panels indicate that endoscopic ultrasound (EUS) with cyst aspiration should be considered to try to characterise cysts larger or equal to 2 cm.
It is important to bear in mind that the appearance of a pancreatic cyst on an imaging study does not translate directly into patient management. Appropriate management of an individual with an incidentally discovered pancreatic cyst depends upon multiple factors including age, comorbidities, the individual’s willingness to undergo surveillance or surgery, and family history of pancreatic cancer. Therefore management decisions should be individualised and based on multidisciplinary team discussion.
References
https://cancerimagingjournal.biomedcentral.com/articles/10.1186/s40644-017-0126-4#Sec145
Видео Incidental pancreatic cysts - what we know and what we don't know, Jay Heiken канала International Cancer Imaging Society
Pancreatic cysts are very common in the adult population, and the prevalence increases with age. Pancreatic cysts are identified in 13%-20% of adults undergoing abdominal magnetic resonance imaging (MRI) [1, 2] and in 2.6% of individuals undergoing multi-detector CT [3]. How we deal with these cystic lesions has important implications for both patient care and the expenditure of healthcare dollars.
Most pancreatic cysts discovered incidentally on imaging studies are branch duct intraductal papillary mucinous neoplasms (BD-IPMN). The vast majority are larger than 3cm and have a very low risk of malignancy [4]. Nevertheless, certain imaging features of pancreatic cysts are associated with an increased risk of malignancy. The international consensus guidelines for the management of pancreatic mucinous neoplasms [4] identify a group of features which are characterized as “worrisome features” (size larger or equal to 3 cm, thickened enhanced wall, main pancreatic duct (MPD) size 5-9 mm, non-enhanced mural nodule(s), abrupt change in MPD caliber with atrophy of the upstream pancreas, and lymphadenopathy) and “high-risk stigmata” (obstructive jaundice in a patient with a pancreatic head lesion, enhanced solid component, and MPD size larger or equal to 10 mm).
Recent surgical data indicate that individuals with pancreatic cysts may be at increased risk of developing solid pancreatic neoplasms. 4%-10% of patients with resected BD-IPMN are found to have concurrent pancreatic ductal adenocarcinoma [5, 6]. In addition, patients with one or more pancreatic cysts have an increased risk of subsequent development of pancreatic ductal adenocarcinoma [7, 8].
Whether individuals with multifocal BD-IPMN are at increased risk of malignancy is unclear. Although most studies have not shown an increased risk of malignancy compared with solitary BD-IPMN, on study found that in 52 patients with larger or equal to 4 pancreatic cysts, 34% had high grade dysplasia or invasive carcinoma and 17% had a coexistent ductal adenocarcinoma [9].
Almost all of the data available on the biological behavior of pancreatic cysts come from surgical series and longitudinal imaging studies. No randomised controlled trials have been performed. Therefore our approach to the management of incidentally discovered pancreatic cysts is based on consensus guidelines developed by panels of medicine, surgery, pathology and imaging experts [4, 10, 11], and there is still a great deal to be learned about the genetics, natural history and risks associated with these cysts.
All of the consensus guidelines recommend that a cyst larger or equal to 3 cm should be followed as long as it contains no worrisome or high-risk features; however, what the follow-up schedule should be and when surgical intervention is indicated varies among the guidelines. Most consensus panels indicate that endoscopic ultrasound (EUS) with cyst aspiration should be considered to try to characterise cysts larger or equal to 2 cm.
It is important to bear in mind that the appearance of a pancreatic cyst on an imaging study does not translate directly into patient management. Appropriate management of an individual with an incidentally discovered pancreatic cyst depends upon multiple factors including age, comorbidities, the individual’s willingness to undergo surveillance or surgery, and family history of pancreatic cancer. Therefore management decisions should be individualised and based on multidisciplinary team discussion.
References
https://cancerimagingjournal.biomedcentral.com/articles/10.1186/s40644-017-0126-4#Sec145
Видео Incidental pancreatic cysts - what we know and what we don't know, Jay Heiken канала International Cancer Imaging Society
Показать
Комментарии отсутствуют
Информация о видео
23 апреля 2019 г. 15:16:08
00:23:04
Другие видео канала
 Approach to Cystic Lesions of the Pancreas
Approach to Cystic Lesions of the Pancreas The Evolving Role of EUS in Pancreatic Disease — Stephen Kim, MD | UCLA Digestive Diseases
The Evolving Role of EUS in Pancreatic Disease — Stephen Kim, MD | UCLA Digestive Diseases What You Need to Know About Pancreatic Cysts
What You Need to Know About Pancreatic Cysts CT Evaluation of Cystic Pancreatic Masses: A Systemic Approach Part 1
CT Evaluation of Cystic Pancreatic Masses: A Systemic Approach Part 1 What You Should Know About Pancreatic Cysts
What You Should Know About Pancreatic Cysts New Guidelines for Pancreatic Cysts
New Guidelines for Pancreatic Cysts Preoperative diagnosis of pancreatic cysts - Dr. Pitman (MGH) #CYTOPATH
Preoperative diagnosis of pancreatic cysts - Dr. Pitman (MGH) #CYTOPATH Cytomorphologic Review of Pancreatic Fine Needle Aspirations: A Review
Cytomorphologic Review of Pancreatic Fine Needle Aspirations: A Review Update 9: Spectrum of Low-Grade/Cystic Pancreatic Neoplasms and their Management
Update 9: Spectrum of Low-Grade/Cystic Pancreatic Neoplasms and their Management Natural History of Pancreatic Cysts: What Becomes of Them?
Natural History of Pancreatic Cysts: What Becomes of Them? CT Evaluation of Cystic Pancreatic Masses: A Systemic Approach Part 2
CT Evaluation of Cystic Pancreatic Masses: A Systemic Approach Part 2 Mucinous Cystic Neoplasm (MCN) of the Pancreas: What You Need to Know – Part 2
Mucinous Cystic Neoplasm (MCN) of the Pancreas: What You Need to Know – Part 2 Lung Nodules: Four Things to Consider with Bryan Meyers, MD, MPH
Lung Nodules: Four Things to Consider with Bryan Meyers, MD, MPH What are polyps in the colon?
What are polyps in the colon? The Whipple Procedure | Johns Hopkins Medicine
The Whipple Procedure | Johns Hopkins Medicine Why We Haven't Cured Cancer
Why We Haven't Cured Cancer Imaging 101: Immunotherapy Criteria
Imaging 101: Immunotherapy Criteria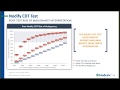 Evaluating lung nodules during the COVID-19 pandemic using blood-based biomarkers
Evaluating lung nodules during the COVID-19 pandemic using blood-based biomarkers What are pancreatic stones and how are they treated?
What are pancreatic stones and how are they treated? Mayo Clinic: John A. Stauffer - Pancreatic Cysts
Mayo Clinic: John A. Stauffer - Pancreatic Cysts