Ulcerative Colitis: Pathophysiology, Symptoms, Risk factors, Diagnosis and Treatments, Animation.
(USMLE topics) Ulcerative Colitis (UC): Signs and symptoms, disease development, pathophysiology, complications, causes, risk factors, diagnosis, and treatments. This video is available for instant download licensing here: https://www.alilamedicalmedia.com/-/galleries/images-videos-by-medical-specialties/gastroenterology-digestive-diseases/-/medias/7e2a23d1-3c6b-4942-a0d2-1418462d1095-ulcerative-colitis-narrated-animation
Voice by: Ashley Fleming
©Alila Medical Media. All rights reserved.
Support us on Patreon and get early access to videos and free image downloads: patreon.com/AlilaMedicalMedia
All images/videos by Alila Medical Media are for information purposes ONLY and are NOT intended to replace professional medical advice, diagnosis or treatment. Always seek the advice of a qualified healthcare provider with any questions you may have regarding a medical condition.
Ulcerative colitis, UC, is one of the 2 major forms of inflammatory bowel disease. In UC, the inner lining of the large intestine is inflamed, causing open sores, or ulcers. UC usually affects only the mucosa and submucosa layers of the intestinal wall.
The condition evolves in the form of recurrent flares, when new lesions form, followed by symptom-free periods of remission, when these lesions heal.
Typical symptoms include abdominal pain and persistent diarrhea, often with mucus and/or blood (rectal bleeding). Some patients may experience fecal urgency, fecal incontinence, or tenesmus – the inability to move bowels in spite of the urge. The disease also often manifests outside the intestine, as a result of inflammation of joints, skin, and eyes. Severe cases can present with systemic symptoms such as weight loss, nausea, vomiting, fatigue and fever.
UC usually starts from the rectum, and may remain limited to that location; or, it can spread upward and affect more of the colon, sometimes the entire colon.
The disease is mildest when it is confined to the lower part of the bowel, in which case the main symptom is blood and mucus in stools, but the stools can be of normal consistency. Once the disease progresses to upper colon, stools become more watery, sometimes consist entirely of blood and mucus. The patient may have multiple bowel movements per day, often with severe cramps and tenesmus.
In the long-term, UC may increase risks for colon cancers, but the most dangerous complication to watch out for is toxic colitis, or fulminant colitis, a life-threatening condition characterized by sudden violent diarrhea, high fever, abdominal pain, and signs of peritonitis. Toxic colitis occurs when inflammation extends into the smooth muscle layer of the intestinal wall, paralyzing the colon muscle. This may lead to colon dilatation, and sometimes perforation.
UC has 2 incidence peaks: one major peak in teens and young adults, and a smaller peak after the age of 50. Some races are more susceptible than others. Family history of the disease is also a risk factor.
Ulcerative colitis is a chronic inflammatory disease, where the ongoing immune response destroys the body’s own tissues. It is associated with abnormally high levels of T-helper cell response, specifically helper T-cell type 2, Th-2. The exact mechanism is not fully understood, but it likely involves both genetic and environmental factors. Multiple genes are identified, most of which act in the immune system, or in maintaining the gastrointestinal epithelial barrier. A mutation in any of these genes may weaken the body’s ability to regulate the extent of immune responses, or to differentiate between self and non-self. An appropriate inflammatory response against a pathogen may get out of control and become chronic; or, the body may mount an inappropriate response against its own antigens.
Involvement of environmental factors is evidenced by higher rates of UC in developed countries, especially urban areas. Interestingly, smoking seems to have a protective effect.
Diagnosis is mostly based on symptoms, but tests are done to exclude other causes: stool tests to exclude infections, colonoscopy to rule out cancers.
Treatments include:
Dietary management to maintain good nutrition but avoid foods that may cause discomfort.
Diarrhea medications to relieve symptoms, except in case of severe attacks.
Mild to moderate patients are prescribed topical or oral 5-Aminosalicylic acid, depending on the affected locations.
Extensive UC is treated with corticosteroids, immunomodulators and biologics.
Severe cases are hospitalized and managed with intravenous corticosteroids; patients are observed closely for development of toxic colitis.
Toxic colitis is treated with high-dose intravenous corticosteroids and antibiotics, and may require emergency surgery.
Some patients with extensive disease may ultimately need surgery to remove the affected part of the colon. Surgery essentially cures the disease.
Видео Ulcerative Colitis: Pathophysiology, Symptoms, Risk factors, Diagnosis and Treatments, Animation. канала Alila Medical Media
Voice by: Ashley Fleming
©Alila Medical Media. All rights reserved.
Support us on Patreon and get early access to videos and free image downloads: patreon.com/AlilaMedicalMedia
All images/videos by Alila Medical Media are for information purposes ONLY and are NOT intended to replace professional medical advice, diagnosis or treatment. Always seek the advice of a qualified healthcare provider with any questions you may have regarding a medical condition.
Ulcerative colitis, UC, is one of the 2 major forms of inflammatory bowel disease. In UC, the inner lining of the large intestine is inflamed, causing open sores, or ulcers. UC usually affects only the mucosa and submucosa layers of the intestinal wall.
The condition evolves in the form of recurrent flares, when new lesions form, followed by symptom-free periods of remission, when these lesions heal.
Typical symptoms include abdominal pain and persistent diarrhea, often with mucus and/or blood (rectal bleeding). Some patients may experience fecal urgency, fecal incontinence, or tenesmus – the inability to move bowels in spite of the urge. The disease also often manifests outside the intestine, as a result of inflammation of joints, skin, and eyes. Severe cases can present with systemic symptoms such as weight loss, nausea, vomiting, fatigue and fever.
UC usually starts from the rectum, and may remain limited to that location; or, it can spread upward and affect more of the colon, sometimes the entire colon.
The disease is mildest when it is confined to the lower part of the bowel, in which case the main symptom is blood and mucus in stools, but the stools can be of normal consistency. Once the disease progresses to upper colon, stools become more watery, sometimes consist entirely of blood and mucus. The patient may have multiple bowel movements per day, often with severe cramps and tenesmus.
In the long-term, UC may increase risks for colon cancers, but the most dangerous complication to watch out for is toxic colitis, or fulminant colitis, a life-threatening condition characterized by sudden violent diarrhea, high fever, abdominal pain, and signs of peritonitis. Toxic colitis occurs when inflammation extends into the smooth muscle layer of the intestinal wall, paralyzing the colon muscle. This may lead to colon dilatation, and sometimes perforation.
UC has 2 incidence peaks: one major peak in teens and young adults, and a smaller peak after the age of 50. Some races are more susceptible than others. Family history of the disease is also a risk factor.
Ulcerative colitis is a chronic inflammatory disease, where the ongoing immune response destroys the body’s own tissues. It is associated with abnormally high levels of T-helper cell response, specifically helper T-cell type 2, Th-2. The exact mechanism is not fully understood, but it likely involves both genetic and environmental factors. Multiple genes are identified, most of which act in the immune system, or in maintaining the gastrointestinal epithelial barrier. A mutation in any of these genes may weaken the body’s ability to regulate the extent of immune responses, or to differentiate between self and non-self. An appropriate inflammatory response against a pathogen may get out of control and become chronic; or, the body may mount an inappropriate response against its own antigens.
Involvement of environmental factors is evidenced by higher rates of UC in developed countries, especially urban areas. Interestingly, smoking seems to have a protective effect.
Diagnosis is mostly based on symptoms, but tests are done to exclude other causes: stool tests to exclude infections, colonoscopy to rule out cancers.
Treatments include:
Dietary management to maintain good nutrition but avoid foods that may cause discomfort.
Diarrhea medications to relieve symptoms, except in case of severe attacks.
Mild to moderate patients are prescribed topical or oral 5-Aminosalicylic acid, depending on the affected locations.
Extensive UC is treated with corticosteroids, immunomodulators and biologics.
Severe cases are hospitalized and managed with intravenous corticosteroids; patients are observed closely for development of toxic colitis.
Toxic colitis is treated with high-dose intravenous corticosteroids and antibiotics, and may require emergency surgery.
Some patients with extensive disease may ultimately need surgery to remove the affected part of the colon. Surgery essentially cures the disease.
Видео Ulcerative Colitis: Pathophysiology, Symptoms, Risk factors, Diagnosis and Treatments, Animation. канала Alila Medical Media
Показать
Комментарии отсутствуют
Информация о видео
Другие видео канала
 Ulcerative Colitis Diet, Treatment, Symptoms Flare Up | Nursing NCLEX Review
Ulcerative Colitis Diet, Treatment, Symptoms Flare Up | Nursing NCLEX Review Crohn's Disease: Pathophysiology, Symptoms, Risk factors, Diagnosis and Treatments, Animation.
Crohn's Disease: Pathophysiology, Symptoms, Risk factors, Diagnosis and Treatments, Animation. Management of Ulcerative Colitis | UCLA Digestive Diseases
Management of Ulcerative Colitis | UCLA Digestive Diseases Irritable Bowel Syndrome: Pathophysiology, Symptoms, Causes, Diagnosis and Treatment, Animation
Irritable Bowel Syndrome: Pathophysiology, Symptoms, Causes, Diagnosis and Treatment, Animation Colon Cancer: Pathology, Symptoms, Screening, Cause and Risk Factors, Animation
Colon Cancer: Pathology, Symptoms, Screening, Cause and Risk Factors, Animation What is Ulcerative Colitis?
What is Ulcerative Colitis? Natural Remedies for Colitis | Swami Ramdev
Natural Remedies for Colitis | Swami Ramdev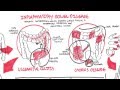 Inflammatory Bowel Disease - Crohns and Ulcerative Colitits
Inflammatory Bowel Disease - Crohns and Ulcerative Colitits Ulcerative Colitis: Do This...
Ulcerative Colitis: Do This... Diverticulitis Signs & Symptoms (And Why They Occur)
Diverticulitis Signs & Symptoms (And Why They Occur) What is Crohn's Disease?
What is Crohn's Disease? Alcoholic Liver Disease, Animation
Alcoholic Liver Disease, Animation Nutrition for IBD (Crohn's and Colitis) Featuring Anne-Marie Stelluti | GI Society
Nutrition for IBD (Crohn's and Colitis) Featuring Anne-Marie Stelluti | GI Society Inflammatory Bowel Disease - Pathophysiology and Complications
Inflammatory Bowel Disease - Pathophysiology and Complications Ulcerative Colitis versus Crohn's Disease, Animation
Ulcerative Colitis versus Crohn's Disease, Animation Anaphylaxis, Animation
Anaphylaxis, Animation In My Words: Life with Ulcerative Colitis | Jacklyn’s Story
In My Words: Life with Ulcerative Colitis | Jacklyn’s Story Inflammatory Bowel Disease ; Crohns Disease and Ulcerative Colitis by Dr. Devesh Mishra
Inflammatory Bowel Disease ; Crohns Disease and Ulcerative Colitis by Dr. Devesh Mishra Crohn's disease (Crohn disease) - causes, symptoms & pathology
Crohn's disease (Crohn disease) - causes, symptoms & pathology Ulcerative colitis - causes, symptoms, diagnosis, treatment, pathology
Ulcerative colitis - causes, symptoms, diagnosis, treatment, pathology